Safe Patient Handling and Movement: Early Mobility in the ICU and the Role of Therapists
| August 2013Early Mobility in the ICU and the Role of Therapists
 Early mobility in the intensive care unit is a hot topic for therapists working in acute care. Recently, with help from the ICU nursing staff, therapists have been assisting patients out of bed and in exercise and mobility routines earlier during their recovery than previously thought possible. Why? Because a growing body of evidence is pointing to the safety, feasibility, and potential benefits of early mobilization in critical and acute care settings.1,2 In consideration of the recognized clinical complications from prolonged bed-rest, early mobility offers a hopeful solution to decreasing the morbidity and lengthy hospital stays of patients in the ICU.
Early mobility in the intensive care unit is a hot topic for therapists working in acute care. Recently, with help from the ICU nursing staff, therapists have been assisting patients out of bed and in exercise and mobility routines earlier during their recovery than previously thought possible. Why? Because a growing body of evidence is pointing to the safety, feasibility, and potential benefits of early mobilization in critical and acute care settings.1,2 In consideration of the recognized clinical complications from prolonged bed-rest, early mobility offers a hopeful solution to decreasing the morbidity and lengthy hospital stays of patients in the ICU.
For many years, deep sedation and bed rest have been considered routine medical care for patients in the ICU. But now clinicians are recognizing that prolonged bed rest results in additional health consequences that further delay recovery from critical illness. These can include debilitating pulmonary issues, decreased cardiac capacity, thromboembolic disease, decreased venous function, orthostatic intolerance, disuse muscle atrophy, joint contractures, decreased bone density and pressure ulcers.
The consequences to the neuromuscular system, however, are of particular concern. It is now understood that prolonged bed rest plays a role in the pathogenesis of neuromuscular weakness in these critically ill patients.1 This muscle weakness in the critically ill is a direct consequence of physical inactivity and can be explained physiologically.3 In ICU survivors, this weakness can persist for years after hospital discharge.4 Because of the prevalence of this phenomenon it now has an acronym: CINMA, for “critical illness neuromuscular abnormalities.5”
By acknowledging the adverse effects of prolonged bed rest and recognizing the positive research outcomes in early mobility,2 hospitals are responding accordingly.6 Deep sedation is being reduced and mobilization protocols are put in place soon after a patient is admitted to the ICU.2 “Studies are showing that those patients who achieve ambulation >4000 steps have a better prognosis and fewer complications,” says Anna K. Steadman, MA, OTR, CHSP, the owner of Essential Ergonomics, LLC in Kyle, TX, a safe patient handling and movement consultant firm.
Because early mobility notably improves functional outcomes,7,8 many therapists are realizing just how important opportunities for physical activity are to quality care in the ICU. Physical therapists and occupational therapists now work as part of a multi-disciplinary team in the ICU to facilitate early exercise and mobilization of patients who are still critically ill or on mechanical ventilation. Clinical trials have shown that a high percentage of these patients are able to successfully ambulate within a safe and well-monitored program.9
Benefits of physical rehabilitation in the ICU include improved peripheral and respiratory muscle strength, improved physical function and mental clarity, decreased dependence on a ventilator, and shorter ICU stay.10-13 Additionally, early mobility has been connected with reduced hospital re-admissions.14 One research study even pointed out that early mobility has the potential to decrease hospital costs secondary to reduced length of stay and hospital re-admissions.15
“Early mobility is taking off across the country” says Margaret Arnold, PT and safe patient handling coordinator of McLaren Bay Region hospital in Bay City, MI. “This typically occurs with up to 3-5 staff assisting the patient for ambulation, with or without a walking device, depending on the patient’s size and ability. Use of safe patient handling equipment can assist in the safety of these activities, as well as allow heavier and more dependent patients to be safely mobilized. There may also be an additional benefit in fewer people being required to safely perform these activities. The research on this hasn’t been done yet.”
In the context of mobilizing patients early, safe patient handling (SPH) equipment is extremely important as it plays a role in keeping both the patient and caregiver safe when attempting mobility and transfers. Patients in critical or acute care may be large, unsteady, or not fully alert. As Kathleen Rockefeller, PT, ScD, MPH and faculty member of Nova Southeastern University’s DPT program says, “A patient may be fully coherent in the morning and really tired in the evening, or their pain medications may differ, or other medications or treatments may change. The patient is not static. We have to be prepared that the patient’s condition may change continuously. For this reason it is important for the therapist to evaluate patient factors and to consider appropriate use of safe patient handling and movement equipment for transfer and mobility of the patient.” Not only will appropriate equipment maintain the safety of the patient and therapist during patient mobilization and transfers, but also enable ambulation of patients with less staff assistance, contributing to better utilization of staff resources. As Margaret Arnold concludes, “Applying safe patient handling to early mobility in the ICU can enable staff to more safely implement the evidence-based practice with larger clients.”
However, as early mobility is still in its pilot stages, not every facility is aware of the availability of this equipment. Anna Steadman, MA, OTR, CHSP, owner of Essential Ergonomics, LLC, notes “To make early ambulation a reality in ICU and acute care settings, we need to get the knowledge out there that technology exists to assist clinicians to safely ambulate patients earlier in their stay.”
Manufactures of safe patient handling equipment in their turn are working to meet the demands of this new market. Therapists can play a role in designing this equipment by providing feedback on what changes or functions might better meet the safe patient handling needs of both them and their patients. “The manufacturers want to hear our feedback,” says Kathleen Rockefeller, PT, ScD, MPH. “They really welcome our ideas, such as concepts for modifications to existing products that would make them more useful. Or, input for products that may not be developed yet, that we think would serve a role in the patient-handling continuum.”
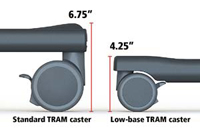
Take for example the Rifton TRAM. This SPH device was created in response to requests from therapists for a low profile transfer and mobility device. The TRAM combines three unique functions into one device: seated transfers, sit-to-stand transfers and gait training. Because of its versatility, the TRAM is being used in a wide variety of settings including schools, hospitals, rehab facilities, skilled nursing facilities, and intermediate care facilities for a variety of transfer and mobility needs.
Safe patient handling and active patient mobilization, although critical in the ICU, cannot be confined to this setting only. Physical activity needs to continue throughout the hospital stay and into the community. “We need to push for maximizing mobility across the continuum of care,” says Margaret Arnold, PT. “Are we mobilizing all patients to the optimal degree? We must continue to promote their mobility once they are discharged from critical care – from the nursing unit, to sub-acute, rehab, skilled nursing, long term care, and at home.”
With increasing interest in early mobility and the emerging scientific evidence supporting this approach, mobility protocols are rapidly being implemented across the United States in many clinical settings. As a result, safe patient handling and movement is receiving much needed attention. Combining early mobilization with safe patient handling certainly results in increased benefits to patient health and mobility and positive rehabilitation outcomes.
References
1. Truong AD, Fan E, Brower RG, Needham DM. (2009) Bench-to-bedside review: mobilizing patients in the intensive care unit – from pathophysiology to clinical trials. Critical Care 13:216 doi:10.1186/cc7885 Full Text
2. Needham DM. (2008) Mobilization patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA 300(14):1685-90. doi: 10.1001/jama.300.14.1685. Abstract
3. Chambers MA, Moylan JS, Reid MB. (2009) Physical inactivity and muscle weakness in the critically ill. Crit Care Med 37(10 Suppl):S337-46. Abstract
4. Fletcher SN, Kennedy DD, Ghosh IR, Misra VP, Kiff K, Coakley JH, Hinds CJ. (2003) Persistent neuromuscular and neurophysiologic abnormalities in long-term survivors of prolonged critical illness. Crit Care Med 31(4):1012-1016. Abstract
5. Stevens RD, Dowdy DW, Michaels RK, Mendez-Tellez PA, Pronovost PJ, Needham DM. (2007) Neuromuscular dysfunction acquired in critical illness: a systemic review. Intensive Care Med 33:1876-1891. Abstract
6. Korupolu R, Gifford JM, Needham DM. Early mobilization of critically ill patients: reducing neuromuscular complications after intensive care. (2009) Contemporary Critical Care. 6(9):1-12.
7. Brahmbhatt N, Raghavan M, Milbrandt EB. (2010) Early mobilization improves functional outcomes in critically ill patients. Critical Care 14(5):321. Abstract
8. Adler J, Malone D. (2012) Early mobilization in the intensive care unit: a systematic review. Cardiopulm Phys Ther J. 23(1):5-13. Abstract
9. Kress JP. Clinical trials of early mobilization of critically ill patients. (2009) Crit Care Med. 37(10 Suppl):S442-S447. Abstract
10. Kayambu G, Boots R, Paratz J. (2013) Physical Therapy for the Critically Ill in the ICU: A Systematic Review and Meta-Analysis. Crit Care Med 41(6):1543-54. doi: 10.1097/CCM.0b013e31827ca637. Abstract
11. Needham DM, Korupolu R, Zanni JM, Pradhan P, Colantuoni E, Palmer JB, Brower RG, Fan E. (2010) Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Archives of Physical Medicine and Rehabilitation 91(4): 536-542. Abstract
12. Needham DM, Korupolu R. (2010) Rehabilitation quality improvement in an intensive care unit setting: implementation of a quality improvement model. Top Stroke Rehabil. 17(4):271-81. doi: 10.1310/tsr1704-271. Abstract
13. Stiller K. (2013) Physiotherapy in Intensive Care. An Updated Systematic Review. Chest. May 30. doi: 10.1378/chest.12-2930. [Epub ahead of print] Abstract
14. Morris PE, Griffin L, Berr M, Thompson C, Hite RD, Winkleman C, Hopkins RO, Ross A, Dixon L, Leach S, Haponik E. (2011) Receiving Early Mobility During an Intensive Care Unit Admission is a Predictor of Improved Outcomes in Acute Respiratory Failure. The American Journal of the Medical Sciences. 341(5):373-377. Abstract
15. Lord RK, Mayhew CR, Korupolu R, Mantheiy EC, Friedman MA, Palmer JB, Needham DM. (2013) ICU early physical rehabilitation programs: financial modeling of cost savings. 41(3):717-24. Abstract